Walking is one of the most natural movements we perform, yet it involves a complex interplay of muscles, joints, and neurological signals, prompting the question “What is an abnormal walking gait?”. When this harmony is disrupted, it can lead to an abnormal walking gait, impacting mobility and overall well-being. Recognizing the signs, causes, and solutions is key to addressing gait issues and maintaining a healthy, confident stride.
Understanding Your Walking Gait
Your body moves in a very intricate dance when you walk. This dance is broken down into a series of movements that repeat with each step you take. The sequence of movements is divided into two main phases of your gait cycle:
- Stance Phase: Your foot is on the ground during the stance phase. Your weight-bearing foot is loaded with your body weight. You spend about 60% of your gait cycle in the stance phase, as your foot is on the ground with you most of the time.
- Swing Phase: Your foot is off the ground during the swing phase. This is when your leg is preparing to move forward to the next position. While one foot is swinging through the gait cycle, your opposite foot is getting ready to weight bear.

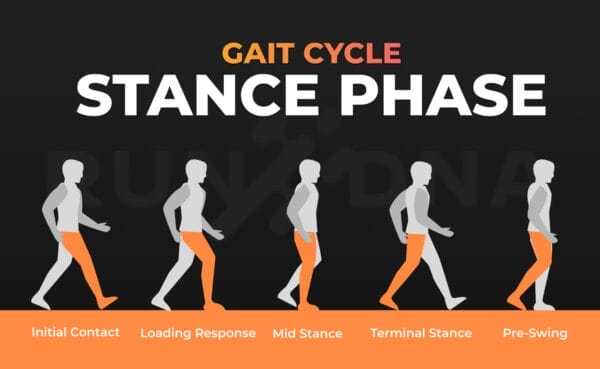
Within these phases, various elements work together – muscles, joints, and your nervous system. Your body is working hard to balance, propel you forward, and absorb shock.
Gait instructors use their eyes and technology to analyze your walking form. We use a gait analysis system, like the one offered by RunDNA, to capture detailed information about your foot strike, stride length, and other gait elements. This information is invaluable to you and your instructor as it helps you identify areas to improve your technique.
What Consitutes a Normal Gait?
A normal gait has three key elements:
- Symmetry: Your legs move in a symmetrical pattern, with your body weight evenly distributed between them.
- Balance: You maintain your balance throughout the gait cycle, not leaning or stumbling.
- Smoothness: Your movements are smooth from one step to the next, without any jerky motions.
Several elements help you maintain a normal gait:
- Muscle Strength: Strong legs, hips, and core muscles help stabilize and propel you forward.
- Joint Flexibility: Adequate hip, knee, and ankle motion is important for a smooth gait.
- Neurological Control: Effective coordination and timing of muscle activity hinge on a well-functioning nervous system.

How Does a Walking Gait Become Abnormal?
An abnormal gait is any pattern of walking that is irregular or different from the normal rhythm and pattern of movement. There are many types of abnormal gaits, and they can be caused by a variety of problems, such as pain, muscle imbalances, neurological disorders, injuries, or many other conditions. Most people limp when they have an abnormal gait, which is often caused by pain in one leg. Stiffness or irregularity in the way your joints move can also create an abnormal gait.
If one or both of your legs drag while you’re walking, you may have a weakened or tight lower extremity. An abnormal gait can also cause you to lean from side to side while you’re walking, which can make you more likely to fall. In some cases, a foot can drag while walking, which is often caused by weakness or tightness in the legs. Other signs of an abnormal gait include:
There are many different types of abnormal gait patterns, and each is associated with specific underlying conditions or problems.
- Antalgic gait: A limp caused by pain that makes you avoid weight-bearing on the affected leg. You’ll shorten the stance phase of your gait on that side to minimize your pain.
- Cerebellar gait: Characterized by a wide-based, unsteady, and staggering walk, often caused by damage or dysfunction in the cerebellum due to conditions like ataxia or stroke.
- Spastic gait: Stiffness and clumsiness in your limbs that causes an irregular, awkward gait. This is often caused by neurological disorders such as cerebral palsy or multiple sclerosis, which then lead to gait disorders.
- Scissors gait: Characterized by the knees and thighs crossing or “scissoring” during walking, often caused by conditions like cerebral palsy or spastic diplegia.
- Hemiplegic gait: Characterized by a stiff-legged, swinging motion of one side of the body, typically caused by weakness or paralysis from conditions like stroke or cerebral palsy.
- Waddling gait: Marked by a side-to-side motion of the hips while walking, often caused by muscle weakness in the hip area, such as in conditions like muscular dystrophy or hip dysplasia.
- Ataxic gait: An unstable, wide-based gait that is often caused by balance problems. You may stagger or lurch while you walk.
- Neuropathic gait: This is marked by high stepping to compensate for foot drop, often caused by peripheral nerve damage or conditions like diabetes-related neuropathy or Charcot-Marie-Tooth disease.
- Propulsive gait (Parkinsonian gait): This type of gait affects people diagnosed with Parkinsonism or Parkinson’s disease.
- Steppage gait: Characterized by exaggerated lifting of the knees to avoid dragging the toes, often caused by weakness or paralysis of the dorsiflexor muscles, commonly seen in conditions like foot drop or peripheral neuropathy.
- Shuffling gait: Defined by small, flat-footed steps with minimal foot clearance, often associated with conditions like Parkinson’s disease or other neurological disorders.
- Myopathic gait: A waddling motion caused by weakness in the hip girdle muscles, often linked to conditions like muscular dystrophy or other muscle disorders.
- Trendelenburg gait: Your pelvis drops down when you stand or walk because your hip muscles are weak. This is often caused by problems with your hip joint or nerve damage.

Common Culprits of an Abnormal Walking Gait
An abnormal gait can be caused by a variety of medical conditions, lifestyle choices, and environmental factors. Often, underlying medical conditions are the primary cause. Neurological disorders such as a stroke, cerebral palsy, and Parkinson’s disease can affect the nervous system’s ability to coordinate smooth and balanced movements. Musculoskeletal problems, such as arthritis, hip dysplasia, and conditions that affect the length of one leg (leg length differences), can affect joints and muscles, causing stiffness and abnormal gait. Conditions such as a malunited fracture or a severe sprain can also affect gait, often due to pain or limited motion in the foot and ankle.
Lifestyle factors and our environment also can play a haunting role in creating an abnormal gait. Poor posture and ergonomics are common culprits, often caused by hours spent sitting in a home or office workspace that promotes poor positioning. Wearing shoes that are poorly made or too short can strain the feet and ankles, causing them to abnormally and painfully adapt. A lack of regular exercise and mobility also can weaken muscles needed to support a normal gait. In many cases, addressing the underlying cause of an abnormal gait is possible with medical treatment, therapy and/or lifestyle changes.
Why Is It Important to Address an Abnormal Gait?
Correcting an abnormal gait is extremely important and can affect many aspects of a person’s life. One of the main concerns is the risk of falls and injury. An abnormal gait can turn something as simple as walking across the room into a dangerous activity, especially for seniors and people with pre-existing health conditions.
Abnormal gait mechanics also puts additional stress on your muscles, joints, and spine. This can lead to chronic pain, inflammation, and deformities over time. Additional complications can develop as your body compensates for the abnormal gait, stressing other parts of your body.
An abnormal gait can also greatly affect your quality of life. Limited mobility can make it difficult to perform daily activities on your own, leading to feelings of frustration and dependence. The social and emotional aspects of an abnormal gait are many and often mirror the physical challenges. Many people are embarrassed or self-conscious about their gait, especially in public. This can cause them to avoid social events and situations, leading to depression and low self-esteem. Fortunately, many abnormal gait patterns can be addressed with early intervention and treatment.
How to Diagnose an Abnormal Walking Gait
Diagnosing an abnormal walking gait involves a combination of clinical assessments and advanced technological tools.
Clinical Assessment
Clinically, healthcare professionals, including physical therapists, orthopedic doctors, and podiatrists, can diagnose gait abnormalities. The first step in evaluation is a thorough observation of the way a patient walks, including their posture and overall mechanics of movement. This is completed during a daily ambulation, as well as with more sophisticated instruments, such as force plates and electronic motion analysis systems.
Additionally, a patient’s strength, flexibility, and overall neurological status (nerve and muscle function) are evaluated. Gait abnormalities can be caused by muscle imbalances, joint restrictions, and/or nerve dysfunctions, among other things. Depending on the clinical suspicion, other diagnostic tests such as X-ray, MRI, or EMG may be ordered. The clinical evaluation is a vital step in developing a treatment plan for an abnormal gait.
Gait Analysis Equipment
A clinical evaluation isn’t the only way to diagnose an abnormal gait—walking gait analysis equipment is used to further evaluate and diagnose the issue. While some clinics use simple video cameras mounted high above the way, more advanced laboratories use extensive systems that track a person’s movement as they walk, run, or jump on a motorized treadmill. RunDNA’s walking gait analysis system uses Helix 3D equipment to reveal underlying gait factors, and it generates reports and personalized programs instantly.
Their system assesses stride length, foot position, and overall efficiency of movement. It can detect slight abnormalities in gait that would go unnoticed by the regular human eye. The feedback the system provides is not generic and allows clinicians to prescribe specific exercises, such as yoga, that complement or correct poor movement patterns. It also allows them to prescribe or recommend the right type of orthotics that fit with a person’s unique gait.
Diagnosing an abnormal gait is the first step in helping people walk with proper technique and reducing the risk of injury and long-term health syndromes.
Treatment Options for an Abnormal Walking Gait
Finding the right treatment for an abnormal walking gait involves understanding the specific needs and challenges of each individual. Options like physical therapy, supportive devices, or medical interventions aim to restore comfort, mobility, and confidence in daily movement.
Physical Therapy and Rehabilitation
- Strengthening Exercises: Target weak muscles to improve stability and support.
- Balance Training: Enhance coordination and reduce the risk of falls.
- Mobility Improvement: Use stretching and range-of-motion exercises to address stiffness and improve flexibility.
- Role of Physical Therapists: Develop customized treatment plans to correct gait patterns and guide patients through effective rehabilitation programs.
Orthotics and Assistive Devices
- Custom Orthotics: Designed to address structural issues like arch problems or leg length discrepancies, promoting proper alignment.
- Assistive Devices: Canes, walkers, and braces improve stability and reduce strain on muscles and joints, making walking safer and more comfortable.
Medical and Surgical Interventions
- Medication: Used to manage pain or inflammation caused by conditions like arthritis.
- Surgery: Addresses severe structural issues; for example, joint replacement surgery can restore mobility and alleviate discomfort in cases of advanced arthritis.
- Rehabilitation Support: Medical or surgical treatments are often paired with physical therapy to optimize recovery and long-term outcomes.
You Can Prevent Abnormal Gait Patterns
Taking care of your overall health is not the theme park thrill ride of lifestyles, but it’s worth the effort. And if you have any abnormal gait patterns or want to avoid obtaining them, taking the right steps to prevent them is an adventure worth embarking on.
Proactive care and paying attention to your daily habits are the first steps towards a balanced gait. Making sure you’re aware of your posture and wearing shoes with adequate arch support are both important to help your body move with efficiency. Poor posture and poorly fitted shoes can lead to imbalances that, over time, can affect your natural gait.
Exercise and stretching are great ways to keep your muscles strong and flexible. Activities that target balance, core strength, and joint mobility are also important to help you maintain a stable gait. Even simple stretches or exercises can help increase flexibility and strength, reducing stiffness and weakness that can lead to abnormal gaits.
If you do experience an injury or notice changes in your gait, it’s important to seek care early on. Many problems that cause pain, swelling, and imbalance can be addressed with simple treatments, preventing more serious conditions from developing. Your primary healthcare provider can help you get back on track quickly and reduce your risk of developing long-term gait abnormalities.
Walk Your Way to Wellness
An abnormal walking gait can impact more than just how you move—it can affect your health, confidence, and quality of life. Understanding its causes and seeking early intervention is key to preventing long-term issues. With tools like gait analysis systems and personalized treatment plans, restoring a natural, comfortable gait is within reach. Taking steps towards understanding what is an abnormal walking gait and focusing on improved mobility today can lead to a healthier, more confident tomorrow.
