Introduction
Plantar foot pain is one of the most common conditions we see in runners and active adults — and one of the most frustrating when it keeps coming back.
The challenge is that plantar foot pain is rarely just a tissue issue. If we focus only on the bottom of the foot without addressing how someone walks, runs, and loads the foot, short-term relief is common. Long-term resolution is not.
Lasting change requires understanding biomechanics, gait mechanics, and load management, not just symptom control.
It’s Not Always “Plantar Fasciitis”
We’ve moved away from calling this condition plantar fasciitis because most persistent cases are not truly inflammatory. Instead, they resemble a plantar fasciopathy, characterized by tissue thickening and reduced blood flow rather than acute inflammation.
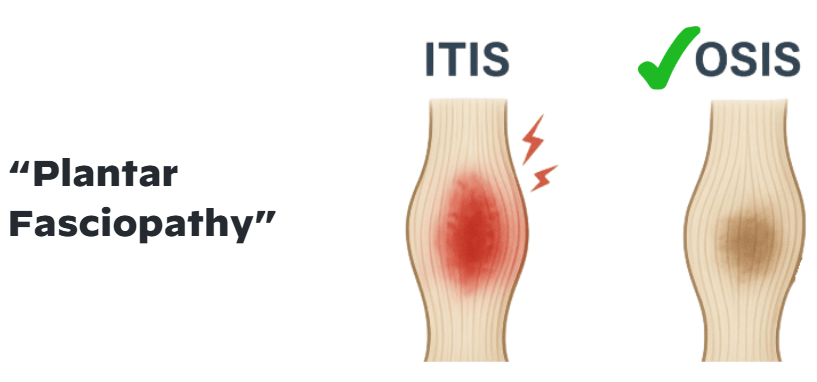
That distinction changes treatment strategy. Instead of simply calming inflammation, the focus shifts to restoring tissue capacity and reducing repetitive strain.
It’s also important to recognize that pain on the bottom of the foot does not automatically equal plantar fascia pathology.
Baxter’s nerve. The calcaneal fat pad. The peroneals. Restrictions at the first ray. Limitations in dorsiflexion. All of these can influence how load is distributed through the foot.
This is why a true differential diagnosis matters.
The Windlass Mechanism and Dynamic Foot Stability
The windlass mechanism plays a central role in how the foot transitions from a mobile adapter to a rigid lever during gait.
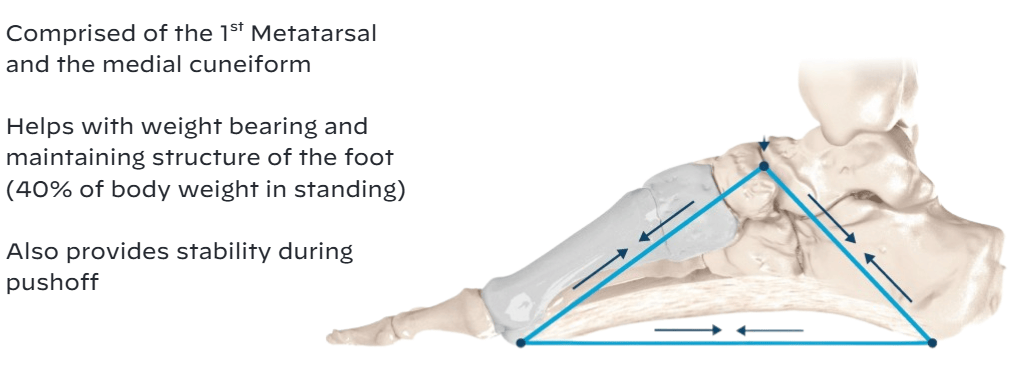
The foot is designed to be dynamic. It adapts to load. When the first ray and medial column fail to move efficiently, tension through the plantar fascia increases. Over time, that increased tension becomes cumulative stress.
If the windlass mechanism isn’t functioning optimally, compensation occurs elsewhere, often without the patient realizing it.
And compensation is where persistent symptoms begin.
Gait Changes Are Often the Missing Link
Once plantar foot pain develops, gait almost always changes, even if the patient doesn’t consciously recognize it. Stride length may shorten as the individual attempts to limit time spent loading the affected foot. Push-off often decreases, particularly through the first ray and great toe, reducing tension through the plantar fascia but also altering how force is transferred forward. Ground contact time may shift between sides, creating asymmetry in loading patterns. Over time, these subtle adjustments redistribute stress throughout the kinetic chain and can prolong strain on the plantar structures or overload neighboring tissues.
These compensations are protective in the short term, but problematic in the long term. When someone unloads the medial column or avoids terminal extension, they often increase stress elsewhere: at the calf complex, the peroneals, or even proximally at the knee and hip. Without identifying and correcting these altered mechanics, symptoms may improve temporarily yet return once normal activity resumes.
That’s why gait analysis is such a critical component of evaluation. If compensatory loading patterns are not addressed, symptoms frequently return, even after pain decreases.
A Comprehensive Treatment Approach
Effective management requires layering interventions strategically rather than relying on a single technique.
Restore Mobility
Restrictions in ankle dorsiflexion or first ray mobility can elevate plantar strain. Targeted manual therapy and mobility work help restore proper mechanics.
Build Strength and Dynamic Stability
The foot intrinsics, toe flexors, calf complex, and peroneals contribute to medial column support. Strengthening these muscles improves load tolerance and reduces passive tissue strain.
Retrain Gait
Subtle adjustments in walking and running mechanics can meaningfully reduce plantar loading. Small changes in cadence, symmetry, and push-off mechanics can shift force distribution.
Use Orthotics Strategically
Orthotics can reduce strain temporarily and allow tissue irritation to calm. However, they should support, not replace, restoring active control.
Incorporate Modalities When Appropriate
Modalities such as extracorporeal shockwave therapy and low-level laser therapy have strong evidence supporting pain reduction and improved function. Reducing pain often allows patients to participate more effectively in strengthening and gait retraining.
Load Management Still Matters
Reducing high-impact volume is often one of the first and most practical steps in managing plantar foot pain. This does not mean complete rest or shutting someone down entirely. Instead, it means temporarily modifying the activities that exceed the tissue’s current capacity. For a runner, that may involve decreasing weekly mileage, reducing intensity, or shifting from speed work to steady aerobic efforts. In some cases, incorporating lower-impact activities such as cycling, swimming, or pool running can maintain cardiovascular fitness while decreasing repetitive strain on the plantar structures.
The goal is not to eliminate load. The goal is to match load to capacity. Plantar fascia tissue, like any connective tissue, responds positively to appropriate stress. Completely unloading the tissue for extended periods can actually delay adaptation and reduce resilience. Progressive loading, introduced gradually and intentionally, helps stimulate tissue remodeling while minimizing flare-ups. This may include structured strength work, controlled walking exposure, and a carefully monitored return-to-run progression.
Consistency matters more than intensity in this process. Small, repeatable exposures to load will build tolerance over time. Sudden spikes in activity, whether through increased mileage, harder sessions, or longer periods on the feet, are often what trigger setbacks. When clinicians help runners understand how to manage volume, frequency, and progression, they empower them to recover while staying active. That balance is what ultimately reduces recurrence and builds long-term durability.
Bringing It All Together
Plantar foot pain has a high recurrence rate when it is treated as an isolated tissue problem. When the focus remains solely on calming irritation at the bottom of the foot, we may reduce symptoms temporarily, but the underlying drivers of load and compensation often remain unchanged. A more durable solution emerges when we zoom out and evaluate the entire system — including foot anatomy, the integrity of the windlass mechanism, observable gait deviations, compensatory movement patterns, overall tissue capacity, and cumulative load exposure. Each of these elements influences how stress is distributed through the plantar structures during walking and running.
When we integrate these factors into assessment and treatment planning, we move from symptom management to movement optimization. A comprehensive, movement-focused strategy does more than reduce pain — it improves how the individual loads, absorbs, and transfers force through the foot. That shift not only shortens recovery time, but also builds resilience, helping patients return to activity with greater confidence and a lower likelihood of recurrence.
Want to See this Framework Applied Clinically?
These principles are explored in greater depth in our webinar, 2 Essential Methods for Managing Plantar Foot Pain, where we walked through real-world clinical application of gait analysis, strengthening progressions, mobility strategies, and modality integration.
Watch the full webinar here.